Macroautophagy, also known as autophagy, is a cellular process that plays a crucial role in removing cellular waste products, including damaged organelles and invading pathogens.
It involves the sequestration of cytoplasmic material in two-membrane vesicles called autophagosomes, which later fuse with lysosomes for the digestion of luminal content.
In addition to its role in proteostasis, autophagy also affects non-proteinaceous macromolecules and entire organelles, such as dysfunctional mitochondria-targeted by mitophagy, and other organelles leading to autophagy, reticulophagy, or pexophagy, as well as invading pathogens (xenophagy).
Autophagy is essential for maintaining organelle turnover and is considered a new hallmark of ageing. With age, there is an age-related decline in autophagy, constituting one of the most important mechanisms of reduced organelle turnover.
In humans, the expression of autophagy-related genes declines with age and decreased autophagy in circulating B and T lymphocytes from ageing donors is accompanied by a reduction of the pro-autophagic metabolite spermidine.
Similarly, in rodents, a progressive deterioration of autophagy has been described for some organs, pleading in favour of the idea that autophagic flux is compromised with age.
Reduced autophagic flux may participate in the accumulation of protein aggregates and dysfunctional organelles, reduced elimination of pathogens, and enhanced inflammation because autophagy eliminates proteins involved in inflammasome and their upstream triggers.
Genetic inhibition of autophagy accelerates the ageing process in model organisms. This process is partially reversible, as illustrated in mice in which autophagy restoration is accompanied by attenuated systemic inflammation and segmental reduction of ageing.
In patients, loss-of-function mutations of genes that regulate or execute autophagy have been causally linked to a broad spectrum of cardiovascular, infectious, neurodegenerative, metabolic, musculoskeletal, ocular, and pulmonary disorders, many of which resemble premature ageing at the histopathological and functional levels.
Stimulation of autophagic flux has been shown to increase healthspan and lifespan in model organisms. For example, increasing autophagy solely in the intestine’s enterocytes increases Drosophila lifespan.
Transgenic overexpression of Atg5 under the control of a ubiquitously expressed promoter is sufficient to extend lifespan and to improve metabolic health and motor function in mice.
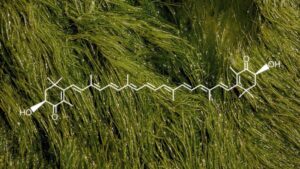
Oral supplementation of spermidine to mice induces autophagy in multiple organs and extends longevity by up to 25%, accompanied by reduced cardiac ageing. Mechanistically, the pro-autophagic effects of spermidine have been linked to an inhibition of the acetyltransferase EP300 or to the hypusination of eIF5A, which is essential for the synthesis of the autophagy transcription factor TFEB.
Pharmacological agents that induce mitophagy and have a positive impact on murine healthspan include NAD+ precursors and urolithin A.
Clinical trials have demonstrated the efficacy of NAD+ precursors in the chemoprevention of non-melanoma skin cancer, in reversing insulin resistance in prediabetic women, and in reducing neuroinflammation in patients with Parkinson’s disease. Moreover, a phase 3 trial has revealed the capacity of urolithin A to improve muscle strength and to reduce C-reactive protein (CRP).
Disabled Macroautophagy
Stem cells are essential for regenerating and repairing tissues in our body. These cells are capable of developing into any other type of cell, making them critical for maintaining healthy organ funct…