Deregulated nutrient sensing refers to the breakdown of the networks that regulate cellular activity, including autophagy, protein synthesis, metabolism, and the formation of mitochondria.
This breakdown occurs as we age, leading to various health issues such as excessive weight gain, glucose dysregulation, and inflammation.
Additionally, inhibition of autophagy may occur, further contributing to cellular dysfunction. The maintenance of healthy nutrient sensing is crucial for the proper functioning of the body and for maintaining healthspan and lifespan.
These networks are called “nutrient sensing” because their activity is highly responsive to nutrition and stress status. In this context, stress status refers to external factors that can impact our body’s ability to metabolize nutrients and maintain metabolic homeostasis.

We can significantly and positively influence MTOR activity through dietary manipulation. Caloric restriction effectively slows biological ageing, primarily because of its impact on MTOR and IGF-1. Other diets that have shown the potential to affect MTOR activity positively include ketogenic diets, low-protein diets, and various forms of fasting.
Our bodies evolved in an environment where the food supply was uncertain, which made our cells evolve to adjust to the availability of nutrients.
The nutrient-sensing systems work to maintain metabolic homeostasis, which is a steady, stable condition.
There are four pathways of nutrient-sensing that regulate metabolism:
- Insulin-like growth factor 1 (IGF-1)
- Mechanistic target of rapamycin (mTOR)
- Sirtuins
- AMP-activated protein kinase (AMPK)
The insulin-like growth factor 1 (IGF-1) pathway is a process in our body that helps us grow and develop. It involves a hormone called growth hormone, which is produced by a gland in our brain called the hypophysis. The growth hormone acts on liver cells to produce IGFs, including IGF-1. IGF-1 then stimulates growth and development in our body.
This pathway is historically implicated in the control of ageing, and inhibition of the GH/IGF-1 pathway in adult or late life extends the lifespan in model organisms, including mice.
Giving female mice a drug that blocks IGF-1 over a long period of time can increase their lifespan, reduce inflammation, and lower the risk of developing tumours.
The mechanistic target of rapamycin (mTOR) pathway regulates cellular metabolism, growth, and proliferation in response to changes in nutrient availability.
Elderly humans are susceptible to viral respiratory infections, and pre-treatment with mTOR inhibitors increased the immune response of elderly volunteers to immunization against influenza and reduced viral respiratory infections in the ensuing winter.
Rapamycin and similar drugs, called rapalogs, have shown the ability to extend lifespan in model organisms by targeting mTOR. By inhibiting mTOR, rapamycin and rapalogs can enhance cellular health and extend lifespan. These drugs have been shown to be effective even when given later in life, making them promising candidates for anti-ageing interventions.
Rapamycin has been extensively studied in mice for its effects on lifespan and healthspan. Various studies have shown that rapamycin can increase the lifespan of mice by up to 23% when administered at a dose that minimizes negative side effects.
Additionally, rapamycin has been shown to improve numerous health markers in mice, including glucose tolerance, insulin sensitivity, and cognitive function.
Rapamycin has also been found to reduce the incidence and severity of age-related diseases such as cancer, cardiovascular disease, and neurodegeneration in mice.
The sirtuins pathway is a family of proteins that regulate many cellular functions, including DNA repair, gene expression, and cell death. They are activated by changes in cellular energy status and are involved in metabolic regulation, stress response, and ageing.
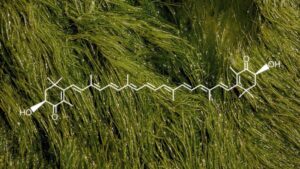
Resveratrol is a plant compound that activates sirtuins and extends lifespan in model organisms.
The AMP-activated protein kinase (AMPK) pathway is a mechanism that senses changes in the energy status of cells. When there is a decrease in the energy currency, ATP, and an increase in AMP, AMPK is activated.
When AMPK is activated, it promotes catabolic processes, such as autophagy and fatty acid oxidation, which can help maintain cellular health and prevent the accumulation of damaged or unnecessary molecules.
Autophagy, in particular, is an important process for removing damaged organelles and proteins, which can lead to cellular dysfunction if not cleared out.
AMPK activation also reduces the synthesis of new molecules, such as proteins and fats, which can help conserve energy and prevent the buildup of excess molecules that can be harmful to the cell.
This shift in cellular processes from anabolic to catabolic is believed to play a role in healthspan and lifespan extension benefits observed in model organisms.
In addition to its effects on cellular metabolism and energy homeostasis, AMPK activation has also been shown to have anti-inflammatory effects, which can contribute to overall healthspan and lifespan extension.
Inflammation is a known driver of many age-related diseases, and by reducing inflammation, AMPK activation may help protect against the development of these diseases.
Overall, the evidence suggests that AMPK activation may play an important role in promoting healthspan and lifespan extension by regulating cellular metabolism, energy homeostasis, and inflammation.
Epigenetic Alterations
Epigenetic alterations occur in the chemical modifications of DNA or the proteins associated with it rather than changes to the DNA sequence itself.
These modifications, also known as epigenetic mark…