
The key to living a longer, healthier life often starts with focusing on sleep.
In the past three decades, the study of sleep has advanced considerably. We now know its impact on our healthspan and longevity. Studies have shown that people who consistently get enough sleep, particularly quality sleep, are more likely to live longer than those who don’t[1].
Sleep dramatically impacts the body’s hormonal, metabolic, and immune systems. These systems play a pivotal role in the development and progression of age-related diseases[2][3][4].
Sleeping well is essential to preserving our cognition as we age and staving off Alzheimer’s disease[5]. It significantly reduces the risk of chronic diseases, helps maintain a healthy weight, reduces obesity risk, and improves our emotional well-being.
Lack of sleep causes the body to generate more cortisol, a stress hormone that can break down skin collagen, the protein that keeps your skin supple and elastic. It also slows the production of human growth hormone (HGH), which fuels the natural tissue repair and rejuvenation process. Low HGH leads to loss of muscle mass, thinning of the skin, and weakening of the bones.
Chronic sleep loss speeds up your ageing clock.
This article first summarises research studies on sleep and longevity. It then details the stages of sleep, how our sleep changes across our life, and concludes with practical considerations that improve our sleep.
In this article
Sleep and Longevity Studies
The Finnish Twin Study
A landmark sleep study was conducted between 1981 and 1984 involving 12,502 pairs of twins.
The study, known as the Finnish Twin Study[6], followed 12,002 pairs of twins over several years, gathering data on their sleep habits and overall health. It was one of the first large-scale studies to examine the relationship between sleep quality and overall health.
The study focused on twins because they provide a unique opportunity to examine the impact of genetics and environmental factors on health outcomes. The twins were surveyed about their sleep habits, including how long they slept each night, how long it took them to fall asleep, and how many times they woke up.
Additionally, the twins were asked about their overall health and any health conditions they had been diagnosed with.
The results were significant: poor sleep quality was associated with a higher risk of various health conditions, including obesity, diabetes, hypertension, and cardiovascular disease. Specifically, the study found that twins who reported poor sleep quality were more likely to:
- Be overweight or obese.
- More likely to have diabetes.
- More likely to have hypertension (that is, high blood pressure).
- More likely to have cardiovascular disease (that is, heart disease).
Researchers observed that those who slept less than seven or more than nine hours per night had a greater chance of dying from all causes. Of the two, short sleepers had the highest risk of early death.
However, the study found that sleep quality was more strongly associated with health outcomes than sleep quantity. In other words, having a high-quality sleep was more important than getting a certain number of hours of sleep each night.
Several long-term studies on the relationship between sleep and health outcomes are considered landmark studies, including:
- The Whitehall II Study
- The Sleep Heart Health Study
- The Nurses’ Health Study
The Whitehall II Study
The Whitehall II Study[7] is a long-term study that began in the 1980s (still ongoing) and has followed over 10,000 British civil servants. The study has investigated a range of health outcomes, including the impact of sleep on cardiovascular disease and mortality.
Some of the key findings are:
- Sleep quantity: The study found that individuals who reported sleeping less than 7 hours per night had a higher risk of developing cardiovascular disease and dying from all causes than those who slept 7-8 hours per night.
- Sleep quality: Poor sleep quality, such as difficulties falling asleep or staying asleep, was found to be associated with an increased risk of developing metabolic disorders, such as diabetes and obesity, as well as a higher chance of dying from all causes.
- Sleep disorders: The study also found that sleep disorders, such as sleep apnea, were common among the participants and were associated with a higher risk of developing cardiovascular disease and dying from all causes.
Overall, the Whitehall II Study highlights the importance of adequate sleep duration and quality to maintain optimal health, reduce the risk of various chronic diseases, and longer life.
The Whitehall II Study
The Whitehall II Study[8] is a long-term study that began in the 1980s (still ongoing) and has followed over 10,000 British civil servants. The study has investigated a range of health outcomes, including the impact of sleep on cardiovascular disease and mortality.
Some of the key findings are:
- Sleep quantity: The study found that individuals who reported sleeping less than 7 hours per night had a higher risk of developing cardiovascular disease and dying from all causes than those who slept 7-8 hours per night.
- Sleep quality: Poor sleep quality, such as difficulties falling asleep or staying asleep, was found to be associated with an increased risk of developing metabolic disorders, such as diabetes and obesity, as well as a higher chance of dying from all causes.
- Sleep disorders: The study also found that sleep disorders, such as sleep apnea, were common among the participants and were associated with a higher risk of developing cardiovascular disease and dying from all causes.
Overall, the Whitehall II Study highlights the importance of adequate sleep duration and quality to maintain optimal health, reduce the risk of various chronic diseases, and longer life.
The Sleep Heart Health Study
The Sleep Heart Health Study (SHHS)[9] is a long-term study that began in 1995 and was completed in 2010. The study collected data on sleep habits, cardiovascular health, and other health factors from over 6,000 participants across several centers in the United States.
Some of the main findings of the SHHS related to sleep quantity and quality are:
- Sleep apnea: Individuals with sleep apnea had a higher risk of developing hypertension, coronary heart disease, and stroke.
- Sleep duration: Short sleep duration (less than 6 hours per night) was associated with an increased risk of hypertension, while long sleep duration (more than 8 hours per night) was associated with an increased risk of coronary heart disease.
- Sleep quality: Poor sleep quality, such as difficulty falling or staying asleep, was associated with an increased risk of hypertension, coronary heart disease, and stroke.
Overall, the SHHS highlights the critical relationship between sleep disorders, sleep quantity and quality, and the risk of cardiovascular disease.
The Nurses’ Health Study
The Nurses’ Health Study (NHS)[10] is a large, long-term cohort study that has investigated various aspects of women’s health since its inception in 1976 (still ongoing).
Some of the main findings of the NHS related to sleep quantity and quality are:
- Sleep duration: The NHS found that both short and long sleep durations were associated with an increased risk of coronary heart disease among women. Specifically, sleeping less than five or more than nine hours per night was associated with a higher risk of heart disease.
- Sleep quality: The study found that poor sleep quality, such as difficulty falling or staying asleep, was associated with an increased risk of developing type 2 diabetes and cardiovascular disease.
- Shift work: The NHS also investigated the impact of shift work on sleep and health outcomes. The study found that working rotating night shifts for several years was associated with an increased risk of developing type 2 diabetes, cardiovascular disease, and certain types of cancer.
The NHS emphasizes the importance of adequate sleep quantity and quality for maintaining optimal cardiovascular and metabolic health, particularly among women. The study also highlights the potential health risks associated with shift work and disrupted sleep patterns.
These landmark and more recent studies have continued to build our understanding of the relationship between sleep quality and health outcomes. They have provided valuable insights into prioritizing high-quality sleep for overall health and longevity.
More recent examples include:
- The Sleep Duration and Mortality Study.
- The Sleep Duration and Cognitive Function Study.
- The Low-Risk Sleep Patterns Study.
The Sleep Duration and Mortality Study
Researchers investigated the relationship between sleep duration and cardiovascular disease (CVD) risk factors among a large cohort of middle-aged and older adults in China[11]. The study was conducted between 2009 and 2012 and included 24,713 participants who were followed up for an average of 6.7 years.
The study found that short and long sleep durations were associated with an increased risk of CVD risk factors, including hypertension, diabetes, and hyperlipidemia (high cholesterol levels and triglycerides). Specifically, sleeping less than 7 hours per night or more than 9 hours per night was associated with an increased risk of these CVD risk factors compared to sleeping 7-8 hours per night.
The study also found that the association between sleep duration and CVD risk factors was stronger in women than men. The findings suggest that maintaining adequate sleep duration, between 7-8 hours per night, may be important for preventing CVD risk factors.
Sleep Duration and Cognitive Function Study
Another Chinese study, conducted between 2009 and 2013, included 2,293 participants aged 65 years or older, found short and long sleep durations were associated with worse cognitive function than sleeping 7-8 hours per night[12].
Specifically, sleeping less than 6 hours or more than 8 hours per night was associated with a more significant decline in cognitive function over time, as measured by memory, attention, and executive function tests.
The study also found that the association between sleep duration and cognitive function was stronger in women than men.
The findings suggest that maintaining adequate sleep duration, between 7-8 hours per night, may be important for preserving cognitive function in older adults, particularly women.
Low-Risk Sleep Patterns Study
The most recent study, presented at the ACC Scientific Session 2023[13] investigated the association between sleep patterns, mortality, and life expectancy among 172,321 adults (average age 50 and 54% women) in the United States.
The study found that individuals who followed “low-risk sleep patterns,” defined as sleeping 7-8 hours per night, not snoring or having insomnia, and being a “morning person,” had a lower risk of death than those who did not follow these patterns.
Specifically, the study found that individuals who followed low-risk sleep patterns had a 66% lower risk of premature death than those who did not. The study found that following low-risk sleep patterns was associated with an increase in life expectancy of 4.7 years for men and 2.4 years for women.
The study further projected estimated gains in life expectancy if good sleep was invested in starting at age 30, of 5.6 to 6.7 years.
Moreover, the study data suggested that about 8% of deaths from any cause could be attributed to poor sleep patterns.
Sleep Stages
Your nighttime sleep is a rhythm inside of a rhythm. You go through four stages of sleep, ideally cycling through them four or five times every night. Each completed cycle lasts about 90-120 minutes.
Since your body performs distinct functions during each stage, it’s crucial for your overall health that you not only reach each stage but also experience them without any interruptions.
Typically the stages are broken down as follows:
Stage 1 (NREM)
This is the transition stage between wakefulness and sleep. You may feel drowsy and relaxed during this stage, and your brain produces alpha and theta waves.
Your eye movement and muscular activity will slow down at this stage. If you’ve ever been drifting asleep and felt an arm or a leg suddenly jolt or twitch, it probably happened during this stage.
Stage 2 (NREM)
This stage is still light sleep and is characterized by decreased heart rate, body temperature, and brain activity – predominantly theta waves, which foster learning, memory, and intuition.
During this stage, theta waves are interrupted by sleep spindles, which are 1-2 second bursts of rapid brain waves thought necessary for learning and memory consolidation.
They are named “spindles” because they resemble a spindle or a piece of thread wound around a stick. Sleep spindles are often followed by sleep K-complexes, commonly referred to as a “spindle-K complex”. K-complexes are sudden high-amplitude waves. Research has suggested that the amplitude and frequency of K-complexes may be related to the strength and quality of memory consolidation during sleep.
Stage 3 (NREM)
This is the beginning of deep sleep, also known as slow-wave sleep or delta sleep.
During this stage, the brain waves slow down even further while your heart and respiration rates decrease dramatically. Your body temperature also drops, and your muscles become completely relaxed.
This is the stage where the human growth hormone is released, which is essential for maintaining the body’s flexibility and resilience, and where the regenerative processes occur.
Additionally, the brain starts to eliminate waste using the glymphatic system, which removes debris from the central nervous system.
DNA repair is also at its peak during this stage. Furthermore, energy surges have been observed during this time, as the body seems to be storing energy for the next day.
If someone were to try and wake you during delta sleep, they’d usually have a hard time doing so.
Stage 4 (NREM)
This is the deepest stage of sleep, where your brain produces mostly delta waves. It is tough to wake up during this stage, and if you are woken up, you may feel disoriented and groggy.
Stages 3 and 4 are now often combined and called S3 sleep. During S3 sleep, the body is in a state of rest and repair.
Stage 5 (REM)
This is the stage of sleep where most dreaming occurs.
Your brain becomes more active, and your eyes move rapidly back and forth. Your muscles become temporarily paralyzed (besides your respiratory and cardiovascular functions), which prevents you from acting out your dreams.
Your brain almost exclusively produces slow, impactful delta waves, which are responsible for making our sleep feel restorative and waking up feeling refreshed.
This stage of sleep is known as REM (Rapid Eye Movement) sleep, named after the rapid movements of the eyes that occur during this phase. As the night progresses, the REM phase of your sleep cycle increases, allowing the brain to carry out crucial maintenance processes that benefit your learning, memory, and mood.
Interruptions during this stage, such as snoring, sudden noises, anxious awakenings, or muscle spasms, can disrupt the brain’s ability to sort through daily events and establish cognitive connections. This can have various consequences, including difficulty focusing, learning, and depression.
Every seven to nine hours of sleep should ideally include one to two hours of deep sleep.
Sleep Deteriorates With Age
Sleep changes throughout our lifespan. As we age, it deteriorates. This is represented below in what’s called a hypnogram:
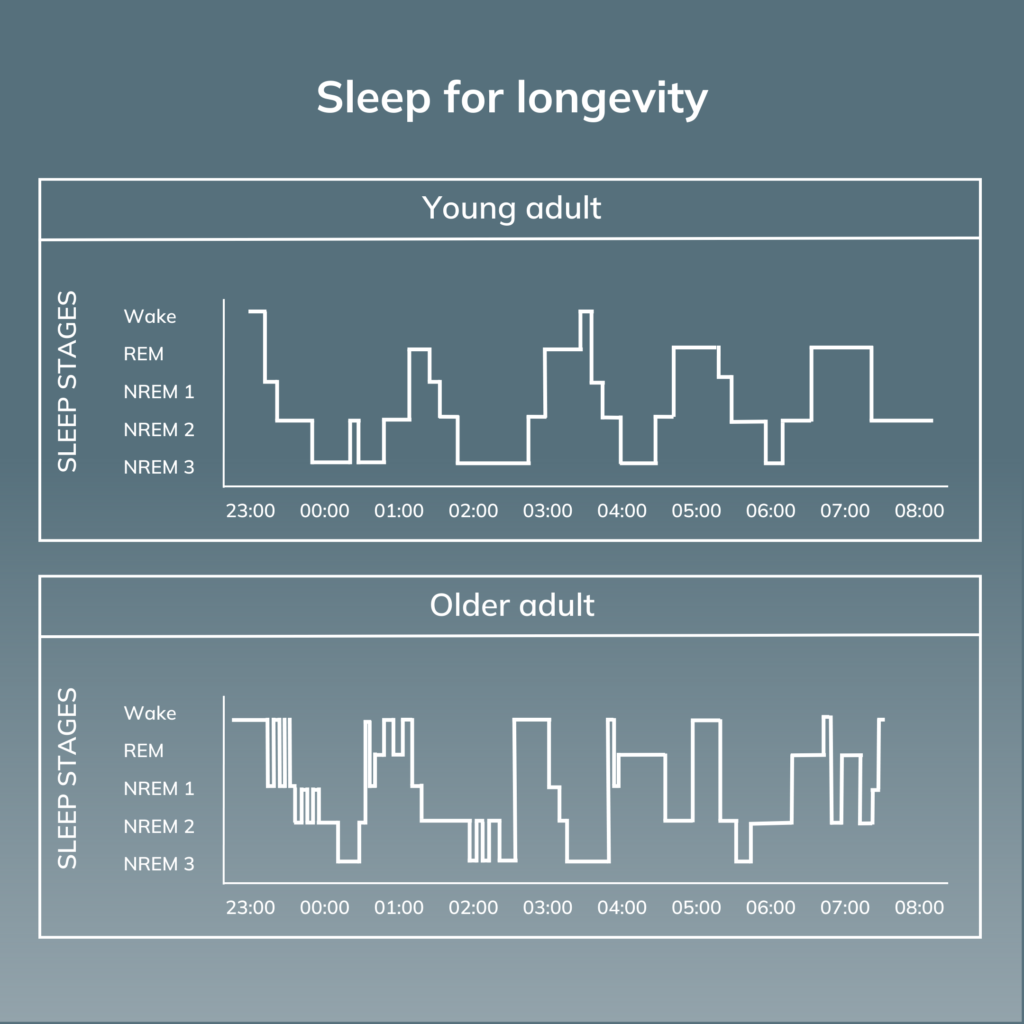
A hypnogram is a graph-based representation of a person’s sleep patterns. Sleep researchers and healthcare providers often use them to evaluate a person’s sleep quality and diagnose sleep disorders.
A hypnogram is divided into vertical bars or segments, each representing a particular stage of sleep. Each segment’s width and height indicates each sleep stage’s duration and intensity. For example, a long, wide segment may indicate a period of deep sleep, while a shorter, narrower segment may indicate a light or REM sleep period.
The hypnogram above shows that young adults typically experience a rhythmic and organized number of sleep phases during the night. The first part of the night is filled with deep sleep (depicted by NREM-3 and NREM-4), while the second half is characterised by increased REM sleep when we’re most likely to dream.
This pattern becomes disrupted in older adults, who experience significant sleep fragmentation. There is less time spent in REM and deep sleep and more time spent awake throughout the night.
Older adults don’t require less quality sleep; their brains can no longer generate it through healthy electrical sleep-related activity.
Not only does the amount of time spent in each sleep stage become disrupted as we age, but the overall quality of sleep also becomes disturbed.
The sleep stages become impaired. The slow waves seen in deep sleep that are responsible for many vital functions are less intense and less dense as we age.
Sleep spindles, a defining feature of NREM sleep, slow down and become less frequent in older people.
Practical Guidance – Tips

If you’re going to unlock the next-level health-enhancing, life-lengthening, all-around-optimizing benefits of sleep, then you’re going to have to start treating a good night’s rest like it matters. Because it does—a lot.
Ensure you get the recommended amount of sleep for adults, 7-9 hours each night[14][15].
Consider taking the following practical tips to help ensure you achieve this duration and, more importantly, improve your sleep quality.
Avoid Screen Usage
Avoid screen time for at least an hour before bed. The blue light emitted by electronic devices can trick our brains into thinking it’s daytime, suppressing the production of the hormone melatonin, which regulates sleep and wakefulness.
If you must use electronic devices before bed, consider using blue light filters or downloading apps that reduce blue light emission to help maintain the natural sleep-wake cycle and improve the overall quality of your sleep.
Wear Blue-Blocking Glasses
Wear blue light-blocking glasses a few hours before bed. Blue blocking glasses can block blue light wavelengths that suppress melatonin production.
Avoid Caffeine
Avoid caffeine at least 6 hours before going to bed.
Consuming caffeine might cause you to go to bed later, sleep for fewer hours overall, and make your sleep feel less satisfying. Additionally, it may cause you to obtain less deep, slow-wave sleep, essential for waking up feeling rested.
By allowing enough time for the body to metabolize and eliminate caffeine, you can minimize its disruptive effects on sleep.
Avoid Alcohol
Avoid consuming alcohol for at least 4 hours before going to bed. While alcohol can initially have a sedative effect and help you fall asleep faster, it can disrupt the quality of your sleep later in the night.
Alcohol can interfere with the normal sleep cycle by reducing the time spent in deep, restorative sleep and increasing the number of awakenings during the night.
It can also increase the likelihood of snoring and sleep apnea, further disrupting sleep quality.
Take a Magnesium Supplement
Magnesium may help to improve sleep by reducing cortisol levels, a hormone that is associated with stress and can interfere with sleep, and by increasing levels of gamma-aminobutyric acid (GABA), a neurotransmitter that helps to promote relaxation and reduce anxiety.
Additionally, magnesium has been shown to help reduce symptoms of restless leg syndrome, a condition that can interfere with sleep quality and duration.
Exercise
Regular exercise has been shown to improve overall sleep quality, reduce the time it takes to fall asleep, increase the amount of deep sleep, and decrease the number of awakenings during the night.
It is recommended that exercise be completed at least 2-3 hours before bed to allow the body to cool down and enter a more relaxed state before sleep. Exercising too close to bedtime may result in difficulty falling asleep or disrupted sleep.
Lower Stress
Lowering stress levels, particularly in the hours leading up to bed, can improve sleep quality and duration. Chronic stress can have a negative impact on the body and mind, contributing to sleep disturbances and insomnia.
When the body experiences stress, the sympathetic nervous system is activated, releasing hormones such as cortisol and adrenaline. These hormones can make it difficult to fall asleep and stay asleep, leading to poor sleep quality and fatigue during the day.
Techniques such as mindfulness meditation, deep breathing exercises, and progressive muscle relaxation have been shown to effectively reduce stress and promote relaxation.
Other stress-reducing activities include regular exercise, leisure time, and socializing with loved ones.
Get Natural Light
Research has shown that individuals who are exposed to natural light during the day experience better sleep quality and duration than those who are not.
It is recommended to aim for at least 30-60 minutes of natural light exposure per day, ideally in the morning or early afternoon.
Exposure to natural light during the day helps regulate the body’s circadian rhythm. This internal biological clock controls sleep and wakefulness.
Watch What and When You Eat
Certain foods and eating habits can disrupt the body’s natural sleep-wake cycle and make falling or staying asleep difficult.
Consuming large meals too close to bedtime can make it more difficult to fall asleep and may contribute to nighttime awakenings.
It is also important to establish regular mealtimes and avoid skipping meals or eating irregularly, as this can disrupt the body’s natural circadian rhythm and contribute to sleep disturbances.
Establish a Consistent Bedtime Routine
Establishing a consistent bedtime routine can improve sleep quality.
A regular sleep routine can help regulate the body’s circadian rhythm, the internal biological clock that controls sleep and wakefulness.
A consistent bedtime routine can involve activities such as taking a warm bath, reading a book, or listening to relaxing music. These activities can help signal the body that it is time to wind down and prepare for sleep.
Additionally, establishing a consistent sleep schedule, with the same bedtime and wake-up time each day (including on the weekend), can help to regulate the body’s circadian rhythm and improve the quality and duration of sleep.
Irregular sleep patterns or frequent changes to sleep schedules can disrupt the body’s natural sleep-wake cycle and make it more difficult to fall asleep or stay asleep.
Boost NAD+ levels
NAD+ is a coenzyme essential for many cellular processes, including energy production and DNA repair. As we age, the levels of NAD+ in our bodies decrease, which can contribute to various age-related conditions and diseases. NAD+ boosters work by increasing the availability of precursors, which the body can use to produce NAD+.
Boosting NAD+ levels may have a positive effect on sleep quality. NAD+ plays a crucial role in regulating the body’s circadian rhythm, which is the natural sleep-wake cycle. As we age, NAD+ levels decrease, which can result in disrupted sleep patterns.
Practice Mindfulness
The choices you make and the activity of your nervous system are closely intertwined, with each greatly influencing the other. Mental well-being impacts family and relationships, daily activities, as…
References





