The human body is a marvel of interconnected systems, and one of the most fascinating is the gut-brain axis. This intricate communication network links the gastrointestinal tract, our gut, with the brain, influencing not only digestion but mood, cognition, and overall health. Recent research has revealed that this axis plays a vital role in maintaining balance within the body and can even impact mental health.
In this article
What’s the gut-brain axis?
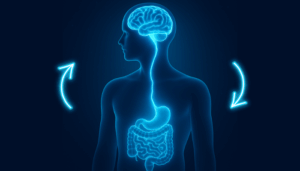
The gut-brain axis (GBA) is a bidirectional communication system connecting the central nervous system (CNS) with the enteric nervous system (ENS), often called the “second brain” due to its ability to function independently. It allows the gut and the brain to send signals to each other, coordinating processes such as digestion, immune function, and emotional regulation.
Key components of the gut-brain axis include:
- Neural Pathways: The vagus nerve is the primary highway for messages between the gut and the brain. It transmits information about gut health, nutrient status, and microbial activity.
- Hormones and Neurotransmitters: The gut produces neurotransmitters like serotonin, dopamine, and gamma-aminobutyric acid (GABA), which play a role in mood and cognition.
- Immune System: Gut microbes influence immune responses, which in turn affect brain function.
- Microbiota: Trillions of bacteria, viruses, and fungi in the gut release metabolites that can signal the brain directly or indirectly.
How Does the Gut-Brain Axis Interact?
The interaction between the gut and brain is complex and multi-layered:
- Neural Communication
The vagus nerve transmits information from the gut to the brain in real-time. For example, the presence of certain nutrients or gut inflammation can trigger neural responses that affect appetite, mood, and even stress levels. - Chemical Messaging
The gut microbiota produces short-chain fatty acids (SCFAs), neurotransmitters, and other metabolites that can cross the blood-brain barrier or influence signaling pathways, affecting emotions, cognition, and behavior. - Hormonal Signaling
Hormones such as cortisol (stress hormone) and ghrelin (hunger hormone) are influenced by gut activity and microbial composition, creating a feedback loop that affects both mental and digestive health. - Immune System Modulation
Gut microbes regulate inflammatory processes. Chronic gut inflammation can release cytokines that reach the brain, potentially influencing mood disorders such as anxiety or depression.
Why It Matters
Understanding the gut-brain axis has revolutionized approaches to health. Conditions such as irritable bowel syndrome (IBS), depression, anxiety, and even neurodegenerative diseases have been linked to disruptions in this communication network. This has led researchers to explore interventions such as probiotics, prebiotics, dietary changes, and stress management techniques to improve gut and brain health simultaneously.
Signs your gut-brain axis needs help
When the gut-brain axis is off balance, it can impact both your mental and physical well-being. Here are some key signs to watch for:
- Bloating, nausea, or acid reflux
- Constipation or diarrhoea
- Stomach cramping or pain
- Worsening of IBS, GERD, or IBD symptoms
- Feeling anxious or irritable easily
- Mental fatigue or sluggishness
- Increased sensitivity to stress
- Loss of appetite or intense cravings
- Feeling low or unmotivated
These symptoms may occur as chronic stress cripples in, which in turn triggers cortisol and slows digestion, leading to bloating, discomfort, and poor nutrient absorption.
Inflammation rises, impairing serotonin and dopamine production, while a weakened gut barrier allows toxins into the bloodstream, causing brain fog and mood swings. Harmful bacteria thrive, further disrupting neurotransmitters and increasing anxiety.
A vicious stress-gut-brain cycle occurs where the imbalanced gut leads to heightened stress responses, and where mental and digestive issues reinforce each other.
What’s affecting your gut-brain axis
- Chronic stress
- Processed and high-sugar diets
- Antibiotic overuse
- Lack of dietary fibre
- Environmental toxins
- Poor sleep
- Excessive alcohol consumption
- Sedentary lifestyle
- Frequent infections or illness
- Artificial sweeteners and additives
When your gut bacteria are disrupted, whether by stress, diet, or lifestyle, it throws off this connection, affecting everything from mood and stress levels to focus and emotional resilience. Balancing the gut microbiome is now recognised as a key step for a healthy nervous system.
5 simple ways to optimise gut-brain connection
Your microbiome is a vast ecosystem of trillions of bacteria, fungi, and other microorganisms living in your gut. The balance between beneficial and harmful microorganisms is what determines your brain function and mental well-being.
Here are a 5 lifestyle changes to make a difference:
1. Move daily
Exercise helps regulate the gut-brain axis. Movement lowers cortisol, improves gut motility, and boosts microbiome diversity. Even a brisk 30-minute walk can support digestion and mood by increasing beneficial gut bacteria and promoting serotonin production. Or simply choose an activity that you enjoy doing everyday. Be it dance, tennis, or football.
2. Optimise your eating habits
Your diet directly impacts how you feel. Fibre-rich foods like vegetables, nuts, and whole grains feed good gut bacteria, while protein supports serotonin production. Avoid excessive sugar and processed foods, which fuel harmful bacteria and increase inflammation. A balanced gut means a balanced mind.
3. Taking high-quality probiotic supplements
Probiotics are one of the most effective ways to rebalance the microbiome, especially when ongoing stress has already disrupted it. It helps in restoring microbial balance, neurotransmitter production, and gut-brain communication.
However, not all probiotics are created equal. The effectiveness of a probiotic depends on several factors.
Refer to this article to understand what is probiotic and how to choose better probiotics.

4. Try relaxation techniques
When you’re stressed, your digestion slows, and your microbiome takes a hit. Try deep breathing, meditation, or yoga to activate the vagus nerve, your gut-brain communication highway. Even a few minutes of mindful breathing can help regulate stress hormones, supporting a calmer mind and healthier digestion.
5. Prioritise sleep
Your gut repairs itself while you sleep. Poor sleep disrupts the microbiome, increases inflammation, and weakens stress resilience. Aim for 7–9 hours of quality rest, keep a consistent bedtime, and reduce screen time before bed to support neurotransmitter production and gut health.
Final Thoughts
The gut-brain axis is one of the most exciting discoveries in modern health science. It shows us that mental and physical health are not separate—but deeply interwoven.
By supporting your gut microbiome through food, movement, stress reduction, and targeted supplementation, you’re not just improving digestion. You’re rewiring your emotional resilience, cognitive clarity, and long-term health.
Nourish your gut, and your brain will follow.