Over the past two decades, one of the most eye-opening medical discoveries has been the realisation that inflammation is not limited to just a few isolated conditions.
Chronic inflammation has quietly become the driving force behind many of the most common health issues today.
In fact, studies reveal that chronic inflammation contributes to over 50% of global deaths—including heart disease, stroke, cancer, and diabetes [1].
What’s even more alarming is that these silent threats often start developing early in life, long before symptoms show up.
Understanding what causes inflammation and how it impacts your health is key to managing or even reversing some of the most serious health risks.
In this Avea article, we’ll dive into the root causes of inflammation, how it affects your body, and what you can do to reduce its impact.
In this article
Free guide to reverse your biological age

- Master the science of rejuvenation.
- Apply proven tips to turn back the clock.
- Transform your health with top longevity specialists.
What is inflammation?
Inflammation is your body’s built-in defence system, a mechanism honed through millions of years of evolution to keep you safe.
It’s how your body fights off harmful invaders like bacteria, viruses, toxins, and injuries.
When your immune system detects a threat, it triggers inflammation to eliminate the danger and start the healing process.
But you know how too much oxygen can kill you? That’s the same with inflammation.
Whilst it’s vital in small, short bursts, when it lingers for too long, it becomes a silent killer. Instead of protecting you, it slowly starts causing damage.
To understand the full picture, let’s break it down into its two main forms: acute and chronic inflammation.
1. Acute inflammation
Acute inflammation is the fast-acting, short-term response your body uses when something harmful is detected. It’s like your body’s immediate reaction to danger, such as when you cut your finger or catch a cold.
Symptoms of acute inflammation
Classic signs of acute inflammation include:
- Swelling: The affected area becomes swollen as immune cells rush in to heal the injury or fight infection.
- Redness and heat: Increased blood flow causes the area to turn red and feel warm.
- Pain or tenderness: Inflammation can trigger pain, either at the injury site or across your body.
- Fever: If the inflammation is widespread (like in infections), your body might raise its temperature to kill off harmful invaders.
Although these symptoms can be uncomfortable, they’re actually signs that your body is doing its job—sending white blood cells and proteins to fight the infection or repair damage.
The great thing about acute inflammation is that it usually resolves itself quickly, leaving your body to heal and return to normal.
2. Chronic inflammation
Now, certain factors can prevent inflammation from resolving. This results in chronic, low-grade inflammation, which is often harder to notice, but much more harmful in the long run.
Unlike the sharp, short bursts of inflammation, this type quietly lingers, affecting your body without any obvious symptoms.
When inflammation becomes chronic, it disrupts your body’s immune tolerance and starts damaging tissues and organs. Over time, this increases the risk of serious health issues.
The effects of chronic inflammation aren’t just limited to adults. If it occurs during pregnancy or childhood, it can have lasting developmental consequences, increasing the risk of chronic diseases later in life.
Symptoms of chronic inflammation
Chronic inflammation is far more insidious. You might not feel or see it happening, but it’s there—slowly chipping away at your health.
Here are some subtle signs to watch out for:
- Persistent fatigue: Feeling constantly tired, even after a good night’s sleep, could be a sign of chronic inflammation.
- Aches and pains: Unexplained joint or muscle pain is often a red flag.
- Weight gain: Struggling to lose weight, especially around your belly? Inflammation could be disrupting your metabolism.
- Digestive issues: Bloating, diarrhoea, or constipation might be signs that inflammation is affecting your gut.
- Frequent infections: If you’re catching colds or infections more often, chronic inflammation may be weakening your immune system.
These symptoms are subtle but persistent—red flags that your body is in a constant state of low-grade inflammation, even if there’s no obvious threat.
Diseases linked to chronic inflammation
Chronic inflammation is one of the 12 hallmarks of ageing. As we age, it becomes more common, which is why older adults tend to have higher levels of inflammatory markers in their blood.
The link between inflammation and disease is undeniable: chronic inflammation acts like a slow poison, increasing your risk for conditions such as:
- Metabolic syndrome (high blood pressure, high blood sugar, and abnormal cholesterol levels)
- Type 2 diabetes
- Non-alcoholic fatty liver disease
- Cardiovascular diseases (heart disease, stroke, hypertension)
- Chronic kidney disease
- Certain cancers
- Depression
- Neurodegenerative diseases (such as Alzheimer’s)
- Autoimmune diseases
- Osteoporosis and sarcopenia (age-related muscle loss)
Chronic inflammation doesn’t just increase the risk of these diseases—it often causes them by breaking down your body’s defences over time. This is why managing inflammation is crucial for long-term health.
The Inflammaging Routine
At Avea, we understand that tackling chronic inflammation and ageing requires more than just surface-level solutions.
That’s why we developed the Inflammaging Routine with a science-first approach, focusing on addressing inflammation from multiple angles, at the cellular and molecular level.
Science-proven ingredients to reduce inflammation

- Reduces chronic inflammation naturally
- Balances gut microbiome health
- Clears harmful senescent cells
- Boosts cognitive and physical health
The Inflammaging Routine is a duo that targets the core drivers of inflammation and ageing:
- Gut health and dysbiosis: An imbalanced gut microbiome is a key contributor to systemic inflammation. Our innovative supplement Biomind was created as a next-generation probiotic specifically to balance the gut microbiome, reducing inflammation at its source.
- Cellular senescence and autophagy: As we age, senescent cells—those “zombie” cells that no longer function properly—accumulate in the body, releasing inflammatory signals. The Avea Cell Primer is formulated to tackle this issue head-on by combining powerful senolytics and antioxidants that clear out these aged cells. It also supports autophagy, the body’s natural cell clean-up process, to help maintain cellular health and reduce inflammation over time.
This combination ensures that both gut health and cellular longevity are prioritised, creating a powerful synergy to not only reduce inflammation, but also boost cognitive and physical health.
Each ingredient was carefully selected for its potency, bioavailability, and ability to work harmoniously with others to deliver optimal results.
By targeting inflammation at the root, Avea’s Inflammaging Routine offers a comprehensive, scientifically-backed way to help manage inflammaging and support healthy ageing.
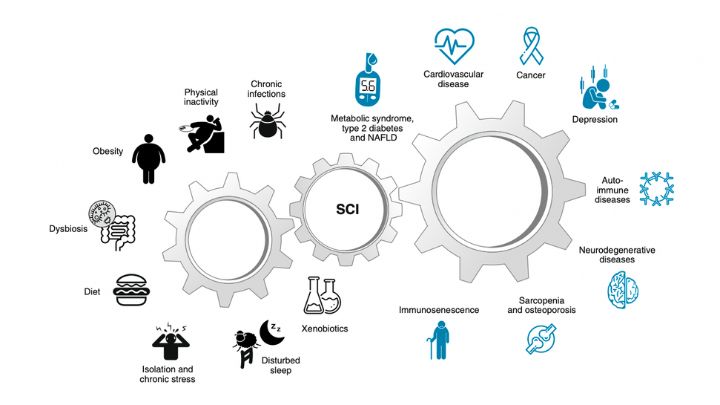
What causes inflammation in your body?
Contrary to popular belief, inflammation isn’t just triggered by infections or injuries. In fact, many aspects of modern life are silently fuelling chronic inflammation in your body—without you even realising it.
From the food you eat to your daily habits, several key factors are driving inflammation in ways that can have serious long-term consequences for your health.
Let’s break down some of the biggest contributors [2].
1. Your diet
What’s on your plate can either be your body’s best friend—or its worst enemy. The typical Western diet, loaded with processed foods, unhealthy fats, and refined sugars, is a major driver of chronic inflammation.
Here’s how it works: diets rich in trans fats, excessive salt, and processed sugars can upset the delicate balance of gut bacteria, leading to a condition known as dysbiosis—an imbalance in your gut microbiome.
This imbalance can increase gut permeability, often referred to as “leaky gut,” which allows harmful substances like toxins and undigested food particles to seep into your bloodstream, triggering inflammation.
Gut health plays a crucial role in controlling inflammation. A healthy gut microbiome acts as a barrier, preventing harmful bacteria and toxins from triggering inflammatory responses.
Some of the biggest dietary culprits for chronic inflammation include:
- Trans fats: Found in processed snacks, baked goods, and fast food, trans fats are known to increase levels of inflammatory markers like C-reactive protein (CRP).
- Refined sugars: Excessive sugar consumption leads to oxidative stress, which activates inflammatory pathways in your body.
- High salt intake: Research shows that high sodium levels skew your immune system toward a more inflammatory state by altering gut bacteria and promoting the production of pro-inflammatory molecules.
In contrast, diets rich in fruits, vegetables, whole grains, and omega-3 fatty acids have been shown to reduce inflammation and improve gut health. Making dietary changes is one of the most powerful ways to keep chronic inflammation at bay.
Learn how to build a longevity diet in 10 simple steps here.
2. A lack of physical activity
In today’s world, we’re moving less than ever. Physical activity has taken a huge toll, particularly in industrialised countries.
New data show that nearly one third (31%) of adults worldwide, that is, about 1.8 billion people, did not meet the recommended levels of physical activity in 2022 [3]. Physical inactivity contributes to 1 in 10 premature deaths worldwide.
Since the COVID-19 pandemic, inactivity has likely worsened, with many of us embracing a “social media and couch” lifestyle, further increasing inflammation without even realising it.
Recent research shows that heavy social media use led to higher levels of chronic inflammation [4].
Surprisingly, this was not just a temporary spike—the inflammation levels remained elevated for five weeks after the initial spike. And where do most people use social media? You guessed it—on the sofa, chair, or bed.
When you exercise, your muscles release special proteins called myokines, which have anti-inflammatory effects throughout the body. When you don’t move enough, your body misses out on these inflammation-fighting benefits.
This inactivity creates a domino effect, leading to insulin resistance, increased levels of inflammatory markers (like C-reactive protein or CRP), and a heightened risk for conditions such as cardiovascular disease, type 2 diabetes, non-alcoholic fatty liver disease, and even certain cancers.
Adults who performed 300 to 599 minutes per week of moderate physical activity (such as walking or weightlifting) had a 26% to 31% lower all-cause mortality and a 28% to 38% lower risk of cardiovascular disease mortality.
Inactivity also contributes to the loss of muscle mass, known as sarcopenia, which further accelerates ageing and inflammation.
Discover how to exercise for longevity—it’s a key factor in managing inflammation and maintaining overall health.
Science-proven ingredients to reduce inflammation

- Reduces chronic inflammation naturally
- Balances gut microbiome health
- Clears harmful senescent cells
- Boosts cognitive and physical health
3. Obesity and visceral fat
Obesity, especially the accumulation of visceral fat (fat around your organs), is a key driver of chronic inflammation. Le’ts get this clear.
Visceral fat is not just excess weight; it acts like an active organ, releasing pro-inflammatory chemicals that can wreak havoc on your body’s systems.
This type of fat produces harmful substances like cytokines and chemokines, which trigger an inflammatory response.
The problem is compounded by insulin resistance, where the body struggles to regulate blood sugar, leading to metabolic syndrome and type 2 diabetes. Dive deeper into why blood sugar spikes are harmful.
Studies have shown that visceral fat also contributes to cardiovascular diseases, non-alcoholic fatty liver disease, and even certain cancers, as it promotes oxidative stress and disrupts normal cellular function.
Losing visceral fat through healthy diet and regular exercise is one of the most effective ways to combat chronic inflammation. Learn how to build an insulin resistance diet here.
4. Unresolved stress
Chronic stress and poor sleep quality have become hallmarks of modern life, but they’re also significant contributors to inflammation.
When you’re stressed, your body releases cortisol, a hormone designed to help you deal with short-term threats.
When stress becomes chronic, elevated cortisol levels can make your body less sensitive to its effects, meaning it can no longer effectively regulate inflammation.
The modern workplace is often a breeding ground for chronic inflammation. High stress, low control environments are literally changing your body’s biochemistry, priming you for higher inflammation levels, disease, and faster ageing.
Over time, this chronic stress contributes to systemic chronic inflammation, weakening your immune system and increasing your risk of diseases like heart disease and diabetes.
Learn how to master stress with Dr. Aditi Nerurkar’s expert guidance.
5. Poor sleep quality
Sleep disruption also plays a major role in causing inflammation. Modern habits, like late-night screen time and exposure to blue light, disrupt your circadian rhythms, making it harder for your body to get the restful sleep it needs.
Research shows that poor sleep quality can directly fuel inflammation, with studies linking it to higher levels of inflammatory markers like C-reactive protein or CRP.
Night-shift workers, for example, who often have disrupted sleep schedules, have been shown to be at higher risk for conditions like metabolic syndrome, type 2 diabetes, and even cancers such as breast and prostate cancer.
Quality sleep is essential for keeping your body’s inflammation levels in check. Discover how to build the best sleep routine.
6. Environmental toxins
In today’s world, we’re surrounded by chemicals and pollutants that simply didn’t exist in the lives of our ancestors.
Most people aren’t aware of just how harmful this constant exposure to modern chemicals can be.
Industrialisation has introduced around 2,000 new substances into the products we use every year—from food and personal care products to household cleaners and even lawn care supplies.
As a result, studies show that over 90% of people have detectable levels of harmful chemicals in their blood.
Chemicals like phthalates, bisphenols, and air pollutants are found in everyday products like plastics, personal care items, household cleaners, and even food packaging.
These chemicals, often called xenobiotics, disrupt your body’s normal functioning and are linked to various health problems. They can act as endocrine disruptors, alter immune function, and promote inflammation.
The rise in exposure to these toxicants correlates with the increasing rates of cardiovascular disease, type 2 diabetes, and even certain cancers.
Tobacco smoke, another major environmental toxin, remains one of the biggest contributors to inflammation. Its toxicants not only damage the lungs, but fuel inflammation throughout the body, leading to a higher risk of diseases like chronic obstructive pulmonary disease (COPD), heart disease, and cancer.
7. Early life events
Did you know that the groundwork for chronic inflammation can be laid down even before you’re born?
It’s called the developmental origins of health and disease—a concept that highlights how early life factors, including those experienced in the womb, shape your long-term risk of inflammation.
Childhood obesity, for example, is a major contributor to chronic inflammation later in life. Obese children often carry inflammation-promoting fat into adulthood, leading to a lifelong battle with metabolic dysfunction and systemic inflammation.
Besides, early-life stress, such as childhood trauma or growing up in a low socioeconomic environment, has been shown to increase inflammation, setting the stage for poor health outcomes in later years.
Interestingly, inflammation can even be passed down through generations. Prenatal exposures—such as a mother’s diet, stress levels, or exposure to environmental toxins—can cause epigenetic changes in the developing foetus.
These changes may alter the baby’s immune system, increasing their likelihood of developing chronic inflammation in childhood and beyond. This is sometimes referred to as “inheriting” inflammation, as these epigenetic changes may persist through generations, influencing not only the child, but also their future offspring.
Research also shows that babies born to mothers with elevated inflammation during pregnancy are at a higher risk of developing conditions like obesity, cardiovascular disease, and neurological disorders later in life.
This transgenerational effect highlights how crucial early life interventions can be in preventing the onset of chronic inflammation-related diseases in adulthood.
8. Chronic infections
Chronic infections, like those caused by viruses such as cytomegalovirus, Epstein-Barr, and hepatitis C, can contribute to systemic chronic inflammation and speed up immune ageing. These infections persist in the body and may interfere with the immune system, promoting long-term inflammation as we age.
For example, cytomegalovirus has been linked to early immune ageing and is a predictor of early mortality. Similarly, HIV accelerates immune ageing, contributing to inflammation-related conditions like heart disease.
Whilst chronic infections are tied to diseases like autoimmune disorders and cardiovascular disease, they interact with factors like environment and genetics.
Interestingly, some non-industrialised societies, such as hunter-gatherers and subsistence farmers, experience high microbial exposure, but show low rates of chronic inflammation. This suggests that whilst infections play a role, lifestyle and environment significantly influence inflammation levels as we age.
9. Cellular senescence
As you age, your body accumulates senescent cells—cells that stop dividing but refuse to die off. These “zombie” cells don’t just sit idle; they actively release pro-inflammatory chemicals, contributing to low-grade chronic inflammation. This inflammation is linked to serious health problems such as heart disease, diabetes, Alzheimer’s, and even cancer.
But here’s the twist: just as senescent cells contribute to chronic inflammation, chronic inflammation itself accelerates the formation of more senescent cells. It’s a vicious cycle where inflammation promotes senescence, and senescent cells, in turn, fuel more inflammation.
The build-up of these senescent cells is triggered by factors like DNA damage, telomere length shortening, oxidative stress, and lifestyle choices such as obesity, chronic infections, and exposure to environmental toxins (e.g., pollution or smoking).
Whilst ageing naturally increases senescence, not everyone experiences the same level of chronic inflammation. This shows that factors like lifestyle, environment, and even genetics play a crucial role in how this harmful cycle unfolds.
So, if you want to break free from the grip of chronic inflammation, addressing both cellular senescence and inflammation is key.
Emerging research on senolytics—compounds that target and eliminate senescent cells—shows promise in reducing the pro-inflammatory effects of these ‘zombie’ cells. Clinical trials are already underway to explore how senolytics could slow ageing and reduce inflammation-related diseases.
Science-proven ingredients to reduce inflammation

- Reduces chronic inflammation naturally
- Balances gut microbiome health
- Clears harmful senescent cells
- Boosts cognitive and physical health
FAQs
To help you quickly find answers to the most common questions about inflammation, we’ve compiled a few quick-fire responses:
- Does drinking alcohol cause inflammation?
Yes, excessive alcohol consumption can cause inflammation. Alcohol irritates your gut lining, promotes “leaky gut,” and increases toxins entering your bloodstream, triggering an inflammatory response. Over time, this can lead to chronic inflammation, raising the risk of liver disease, heart problems, and other inflammatory conditions.
- Does sunflower oil cause inflammation?
Sunflower oil, particularly when highly processed or high in omega-6 fatty acids, can promote inflammation, especially when consumed in excess. Omega-6 fats, when not balanced with omega-3s, may trigger your body’s inflammatory pathways, leading to chronic inflammation.
- Does oat milk cause inflammation?
Oat milk is generally not inflammatory, especially if it’s free from added sugars or unhealthy oils. However, some commercially produced oat milk contains additives or sweeteners that could trigger inflammation, particularly for people sensitive to these ingredients. Discover the benefits of Stevia as a natural sweetener.
- Can exercise cause inflammation?
Yes, intense exercise can cause temporary inflammation as your body repairs muscles. However, regular moderate exercise is anti-inflammatory, reducing chronic inflammation over time and benefiting overall health.
- Does inflammation cause weight gain?
Yes, chronic inflammation can contribute to weight gain. It disrupts metabolic processes, increases insulin resistance, and leads to fat storage, especially around the abdomen. Managing inflammation can help with maintaining a healthy weight. - Does sugar cause inflammation?
Yes, high sugar intake, especially from refined sugars and sugary drinks, can trigger inflammation. Sugar causes spikes in blood glucose, leading to oxidative stress and activation of inflammatory pathways. Over time, this can increase your risk of chronic diseases like diabetes, heart disease, and obesity. - Does dairy cause inflammation?
For most people, dairy does not cause inflammation. However, those who are lactose intolerant or allergic to dairy proteins may experience inflammation in response to consuming dairy products. Symptoms might include digestive discomfort or even systemic inflammation.
- Does gluten cause inflammation?
For people with gluten sensitivity or celiac disease, consuming gluten can trigger inflammation in the gut and beyond. However, for the general population, gluten is not inherently inflammatory. Always check with a healthcare provider if you suspect gluten is causing issues.
- Can dehydration cause inflammation?
Yes, chronic dehydration can contribute to inflammation. Proper hydration helps maintain healthy blood flow and supports the function of organs and tissues. When you’re dehydrated, it can lead to oxidative stress and an increase in inflammatory markers in the body.
Keynote from Avea
Recognising the subtle signs of chronic inflammation is key to preventing long-term damage to your health.
Whilst inflammation is a natural and necessary part of your body’s defence system, it’s important to understand when it becomes harmful.
By making proactive changes to your diet, increasing physical activity, managing stress, improving sleep quality, and reducing your exposure to environmental toxins, you can keep chronic inflammation at bay.
These steps not only protect you from serious health conditions like heart disease, diabetes, and autoimmune disorders, but also improve your overall well-being.
Inflammation doesn’t have to be a long-term health threat—it’s within your power to manage it. Stay informed, be mindful of the signs, and take charge of your health.
References