If you believed that obesity was merely about extra weight and appearance, it’s time for a reality check—it significantly shortens lifespan.
Today, 1 in 8 people worldwide are battling obesity, with global adult rates having more than doubled since 1990.
Even more concerning is the fourfold increase in adolescent obesity in the same period. These numbers represent a critical global health crisis that spans from North America to Southeast Asia.
Whether you’re here for yourself or a loved one, be prepared to be astonished by the deeper implications of this global health challenge.

With over 2.5 billion adults overweight, and 890 million suffering from obesity, the problem is now more than a personal health issue.
Obesity is a burgeoning public health emergency, and governments worldwide need to start changing the way they manage or educate the population.
Whether we consider the impact on life expectancy, the onset of chronic diseases, or the economic burdens on healthcare systems, the weight of obesity is too substantial to ignore.
This article at Avea dives deep into the science of obesity, exploring how it drastically cuts years off lives and what can be done to curb this global epidemic.
Let’s unpack the facts, challenge some myths, and explore effective strategies to enhance longevity in the face of obesity.
In this article
Free guide to reverse your biological age

- Master the science of rejuvenation.
- Apply proven tips to turn back the clock.
- Transform your health with top longevity specialists.
The science of obesity and lifespan
Obesity occurs due to an imbalance between calorie intake and energy expenditure. It can be influenced by a wide array of factors, including
- genetic predisposition
- metabolic rates
- lifestyle choices
- environmental influences
High-calorie diets rich in fats and sugars, combined with sedentary lifestyles, are the most common causes of this energy imbalance.
Genetics also play a crucial role, as certain people may be predisposed to gain weight more easily than others.
But, the environment often exacerbates these genetic risks, especially in settings where high-calorie food is readily available and physical activity is not a routine part of daily life.
Obesity is also affected by socio-economic factors. For instance, lower-income families may have less access to healthy food options or safe places to exercise, increasing their risk of obesity.
Psychological factors such as stress and lack of sleep can also contribute to weight gain, as they may lead to increased appetite and decreased motivation for physical activity.
Defining Obesity
Obesity is medically defined as having an excessive amount of body fat.
This condition is typically assessed using the Body Mass Index (BMI), a straightforward calculation where a person’s weight in kilograms is divided by the square of their height in metres.
According to the World Health Organization (WHO), adults with a BMI of 25 to 29.9 are considered overweight, whilst a BMI of 30 or higher classifies an individual as obese.
It’s important to note that BMI is not a perfect measure—it does not distinguish between weight from fat and muscle, nor does it account for variations in body fat distribution that may occur due to gender, race, or ethnicity.
Increased BMI is closely linked with greater risks of chronic diseases such as type 2 diabetes, cardiovascular disease, and various cancers. These conditions not only diminish life quality, but are also leading contributors to reduced life expectancy.
Those with severe obesity can experience a reduction in life expectancy by up to 14 years.
Prevalence of obesity
Since 1990, the prevalence of obesity has increased dramatically around the globe, a trend that poses significant public health concerns.
In 2022 alone, approximately 1.9 billion adults were overweight, of which over 650 million were obese.
Childhood obesity presents a particularly grim scenario as it tends to carry into adulthood, setting the stage for premature onset of chronic conditions and a lifetime of health challenges.
Internationally, the shift in obesity rates is no longer confined to high-income countries.
Middle- and low-income nations are now seeing similar trends, driven by globalisation and changes in dietary and physical activity patterns.
The availability of high-calorie, nutrient-poor foods has increased globally, whilst sedentary lifestyles have become more common due to technological advancements and urbanisation.
This changing landscape calls for a robust understanding of the science of obesity, which is essential for developing effective public health strategies.
By addressing the root causes and implementing targeted interventions, we can begin to curb this global epidemic and improve life expectancy for future generations.
Diseases and health conditions linked to obesity
Obesity significantly increases the risk of developing a variety of diseases and health conditions, including:
- Cardiovascular diseases:
- Heart disease (such as coronary artery disease)
- Hypertension (high blood pressure)
- Stroke
- Metabolic disorders:
- Type 2 diabetes
- Insulin resistance
- Dyslipidemia (abnormal levels of cholesterol and other fats in the blood)
- Cancers:
- Breast cancer (post-menopausal)
- Colon cancer
- Endometrial cancer
- Esophageal cancer
- Pancreatic cancer
- Kidney cancer
- Respiratory disorders:
- Obstructive sleep apnea
- Obesity hypoventilation syndrome
- Gastrointestinal and Liver Diseases:
- Non-alcoholic fatty liver disease (NAFLD)
- Gastroesophageal reflux disease (GERD)
- Gallstones
- Reproductive health issues:
- Polycystic ovary syndrome (PCOS)
- Infertility
- Complications in pregnancy (such as gestational diabetes and preeclampsia)
- Musculoskeletal Disorders:
- Osteoarthritis
- Gout
- Increased risk of musculoskeletal injuries
- Psychological and neurological conditions:
- Depression
- Anxiety
- Increased risk of certain neurological disorders
As you can see, obesity can impact virtually every system in your body and significantly diminishing both your quality of life and life expectancy.
So, it’s time for a change. And it all begins by educating ourselves.
Prevention strategies
Public health initiatives
The WHO and various national health bodies have initiated several public health policies aimed at reversing this increasing obesity trend.
Initiatives usually focus on:
- improving nutrition education
- enhancing access to healthy foods
- creating more opportunities for physical activity
For instance, some countries have implemented taxes on sugary drinks and unhealthy snacks, whilst others have introduced strict advertising guidelines to limit the marketing of such products to children.
Community programs that encourage active transportation and provide safe and accessible recreational facilities are also crucial. End goal for governments? Creating environments that naturally encourage healthier choices.
Individual lifestyle changes
Both the WHO and the National Institutes of Health (NIH) stress the importance of maintaining a balance between energy intake and energy expenditure to prevent obesity. This involves making informed food choices and increasing physical activity.
Key recommendations include:
- Diet: Incorporating more fruits, vegetables, whole grains, and lean proteins into meals while reducing the intake of high-sugar and high-fat foods. Discover 21 anti-ageing foods you should know about.
- Exercise: Engaging in at least 150 minutes of moderate-intensity or 75 minutes of high-intensity exercise each week, as suggested by health guidelines. Understand why exercising is so important.
- Routine: Establishing consistent eating and activity schedules to help manage weight effectively. Learn how to break bad habits and form good ones.
These changes do not need to be drastic; even small adjustments in daily habits can significantly impact long-term health.
For example, choosing water over soda or taking the stairs instead of an elevator can contribute to better health outcomes.
Obesity treatment options
Medical interventions
The medical management of obesity has evolved significantly, providing several effective options tailored to individual needs.
Current approaches include pharmacological treatments and surgical procedures, both of which have shown promising results in controlling and reducing obesity.
Medications such as Orlistat, Liraglutide, and Bupropion-naltrexone are being prescribed to help reduce appetite or increase feelings of fullness, and are suitable for long-term use under medical supervision.
Meanwhile, surgical options like gastric bypass or sleeve gastrectomy offer more permanent solutions for significant weight loss, particularly in severe cases where other interventions have failed.
These surgical methods have been highly effective, often leading to substantial long-term weight loss and a reduction in obesity-related complications.
Recent advancements in medical treatments offer new hope to those struggling with obesity.
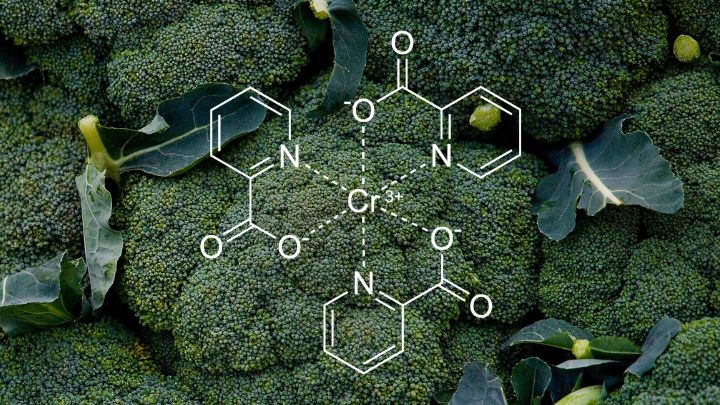
For instance, the development of glucagon-like peptide-1 (GLP-1) receptor agonists has been a breakthrough in obesity pharmacotherapy, significantly improving weight management outcomes and cardiovascular health.
Ozempic, generically known as semaglutide, is a medication that has gained significant attention for its effects on weight loss, although it was originally approved for the treatment of type 2 diabetes.
It belongs to a class of drugs called GLP-1 receptor agonists, which work by mimicking an intestinal hormone that helps control blood sugar, slows down gastric emptying, and affects appetite.
How Ozempic Works
Ozempic functions by stimulating insulin production, reducing the amount of glucose produced by the liver, and decreasing appetite. This trio of effects not only helps manage blood sugar levels, but also contributes to weight loss.
The reduced appetite and slower gastric emptying help individuals feel fuller longer, which can lead to a significant reduction in caloric intake.
Ozempic for weight loss
Though primarily used to manage diabetes, Ozempic has shown promising results in weight management. Clinical trials have demonstrated that when combined with diet and exercise, Ozempic can lead to substantial weight loss.
Considerations and approval
In response to its efficacy in helping with weight reduction, the drug has also been approved at a higher dose under the brand name Wegovy for treating obesity.
It is important for patients considering Ozempic for weight loss to discuss it with their healthcare provider, as it is prescribed specifically for obesity management or weight-related medical problems in individuals with a BMI over a certain threshold.
Side effects and recommendations
Like all medications, Ozempic can cause side effects. The most common ones include gastrointestinal issues such as nausea, vomiting, diarrhoea, stomach pain, and constipation. These effects are generally mild to moderate and tend to decrease over time as the body adjusts to the medication.
Ozempic represents a significant advancement in the treatment of obesity and type 2 diabetes, offering a new hope for individuals struggling with weight management.
However, it should be used under strict medical supervision and in conjunction with lifestyle modifications like diet and exercise to achieve the best outcomes.
Innovative therapies
Research into innovative therapies such as gene editing and microbiome alterations is paving the way for revolutionary changes in obesity treatment.
Gene editing technologies like CRISPR could one day allow scientists to alter DNA sequences that contribute to obesity, potentially eliminating genetic predispositions to excessive weight gain.
Similarly, studies on the human microbiome suggest that altering gut bacteria could significantly affect body weight and metabolism, offering another avenue for effective treatment.
These cutting-edge approaches hold the promise of more personalised and effective obesity treatments.
By targeting the specific genetic and biological factors contributing to an individual’s obesity, these therapies could provide more sustainable solutions and fewer side effects compared to traditional methods.
As research continues, the hope is that these innovative treatments will soon move from experimental stages to become viable options for those in need.
Societal impacts of obesity
Economic burden
Obesity imposes a substantial economic burden on national health systems worldwide.
In the UK alone, the NHS spends over £6 billion annually on obesity-related medical conditions, with broader costs to society, including lost productivity, estimated at around £27 billion each year.
These figures highlight the financial motivation for governments to invest heavily in obesity prevention and management.
Effective interventions not only reduce the strain on healthcare resources, but also enhance workforce productivity by decreasing obesity-related absenteeism and presenteeism.
Investing in preventive measures can yield significant returns, with every pound spent potentially saving several more in future healthcare costs.
Social stigma and mental health
The stigma associated with obesity is pervasive and can significantly impact individuals’ mental health and well-being.
People with obesity often face prejudice and discrimination in various settings, including the workplace, educational institutions, and even within healthcare systems.
This societal bias can lead to psychological distress, reduced self-esteem, and social isolation. There is a pressing need for a shift in societal perceptions, where media and educational campaigns play crucial roles.
By promoting a more inclusive and understanding environment, we can help mitigate the mental health impacts of obesity and encourage those affected to seek help without fear of judgement.
Policy and environment
Urban planning and food industry regulations significantly influence obesity rates. Cities that prioritise bike paths, pedestrian zones, and public parks encourage physical activity among their residents.
Regulating the food industry to limit unhealthy food advertising and reducing the availability of high-calorie, nutrient-poor foods can steer consumer choices towards healthier alternatives.
Policy decisions that make healthy food options more accessible and affordable, coupled with urban environments that promote active lifestyles, are critical in reducing obesity rates.
Such policies need to be supported by government-led initiatives that aim to create healthier communities through strategic planning and regulation. We need a more inclusive society where all individuals can thrive regardless of their body size.
Key note from Avea
Take a stand against obesity today!
Whether you’re an individual, policymaker, or healthcare provider, your actions count. As individuals, embrace a healthier lifestyle through balanced eating and regular physical activity. Share this knowledge with your friends and family.
Policymakers, prioritise and allocate funding to obesity prevention programs that foster healthier communities.
Healthcare providers, emphasise the importance of early intervention and offer comprehensive care to manage obesity effectively.
Together, we can combat this global epidemic, enhancing health outcomes and quality of life for all. Let’s make a collective commitment to turn the tide on obesity.